Pediatric glioma recurrence is a pressing concern in the realm of childhood brain cancer, as the unpredictable nature of these tumors poses significant challenges for pediatric patients and their families. Recent advancements, particularly through the use of artificial intelligence, have sparked hope in accurately predicting the risk of relapse. Researchers at Mass General Brigham have demonstrated that AI can analyze numerous brain scans taken over time, offering a more precise assessment of recurrence than traditional methods. This innovative approach not only aims to alleviate the stress of frequent imaging but also aims to enhance glioma risk assessment, providing tailored treatment strategies. As we delve deeper into the potential of pediatric cancer AI tools, it’s clear that the integration of temporal learning in medicine may revolutionize the way we approach brain cancer management in children.
The recurrence of gliomas in children, a type of brain tumor, presents unique challenges and emotional hurdles for affected families. By employing cutting-edge AI techniques, healthcare professionals are now better equipped to predict the chances of re-emergence in these malignancies. Leveraging advances in medical imaging and temporal analysis, researchers are paving the way for innovative methods in assessing childhood brain cancer risks. This evolving landscape of treatment options underscores the importance of integrating technology into pediatric oncology, emphasizing the need for accurate monitoring and intervention strategies. Embracing these advancements, we can foster renewed hope and enhanced outcomes for children navigating the complexities of pediatric glioma recurrence.
Understanding Pediatric Glioma Recurrence
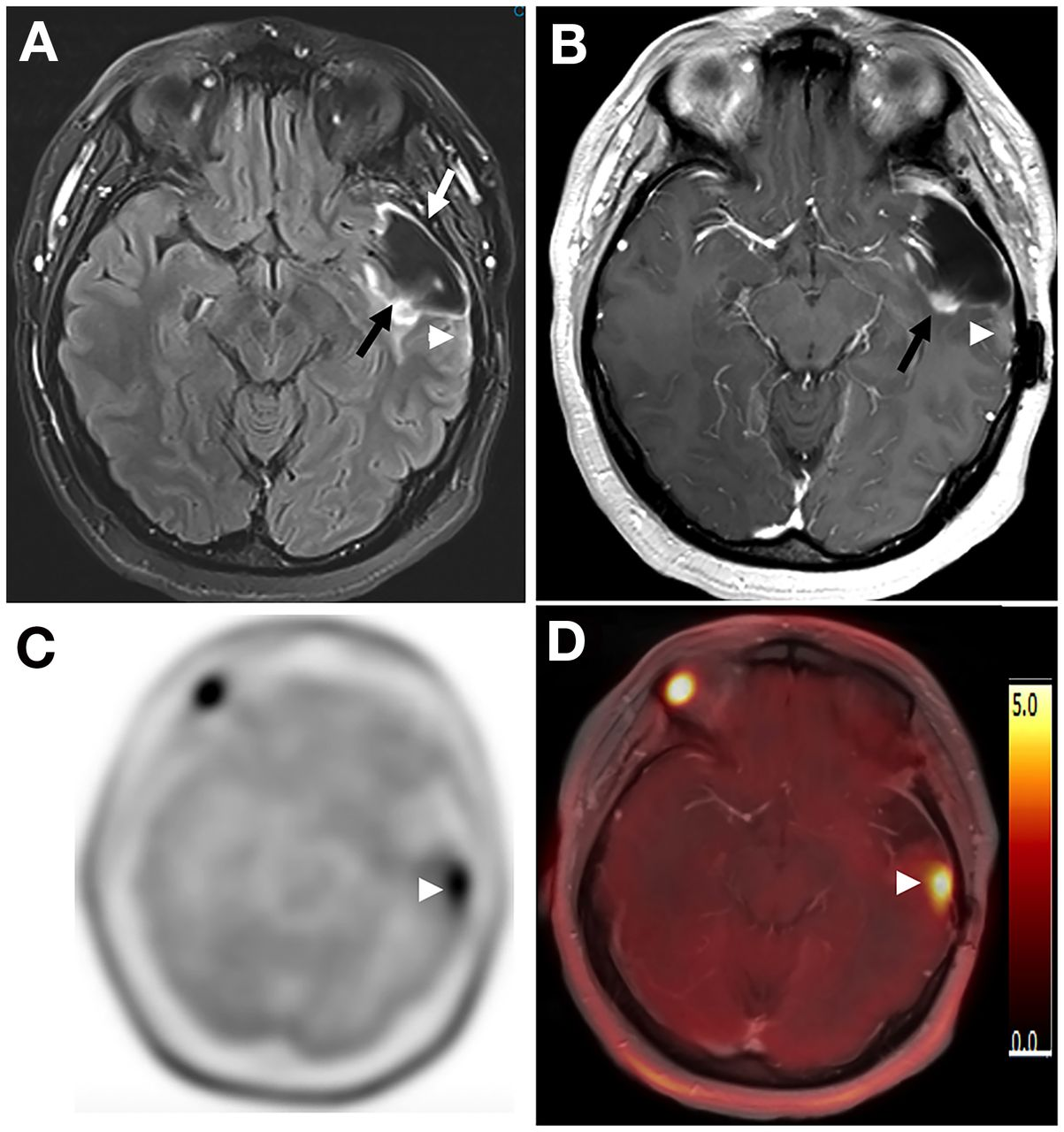
Pediatric glioma recurrence remains a significant concern for healthcare providers and families coping with childhood brain cancer. Gliomas, a type of tumor that originates in the brain or spine, can often be treated effectively with surgery. However, the unpredictability of recurrence presents challenges in treatment planning and long-term prognosis. Traditionally, clinicians relied on single MRI scans to monitor for signs of relapse, a method that proved less than effective in accurately predicting outcomes. As research evolves, understanding the dynamics of recurrence risks becomes crucial for improving care strategies.
Studies show that the risk of recurrence varies significantly among pediatric glioma patients, depending on tumor type and grade. Advances in technology, particularly through the application of artificial intelligence in medicine, have provided new avenues for improving glioma risk assessment. Tools that analyze longitudinal imaging data facilitate early detection of potential relapses, which could lead to timely interventions and better health outcomes for children. With AI’s enhanced predictive capabilities, families can find some relief in knowing that more accurate assessments can lead to more personalized and effective treatment plans.
The Role of AI in Predicting Pediatric Cancer Relapse
Artificial intelligence has emerged as a revolutionary tool in the field of oncology, particularly in pediatric cancer care. Recent studies, such as one conducted by researchers at Mass General Brigham, demonstrate that AI can outperform traditional methods in predicting the risk of relapse in pediatric glioma patients. By analyzing extensive datasets of MRI scans over time, these AI systems utilize patterns and changes in imaging to forecast cancer recurrence with remarkable accuracy. This advancement not only optimizes the monitoring process for patients but also helps to alleviate the emotional burden often placed on families during the post-treatment phase.
The advent of AI-driven predictive models represents a significant breakthrough in managing pediatric brain tumors. Rather than relying on sporadic monitoring through singular MRI scans, AI models equipped with temporal learning techniques analyze trends across multiple imaging sessions. By understanding the progression of gliomas over time, clinicians can identify children who might be at a higher risk for relapse. This proactive approach allows for alterations in treatment plans, either through enhanced vigilance in lower-risk cases or more aggressive therapies for those recognized as high-risk. As the field of pediatric cancer AI tools continues to grow, it instills hope for improved prognostic capabilities in brain cancer management.
Temporal Learning: A New Era for Medical Imaging
Temporal learning in medicine represents a groundbreaking shift in how we approach diagnostic imaging and risk assessment. Unlike conventional methods that assess images in isolation, temporal learning enables the integration of data across multiple time points. This comprehensive approach is especially beneficial for pediatric glioma patients, as it aids in identifying subtle changes that may indicate a likelihood of recurrence. As outlined by researchers from Mass General Brigham, this technique has shown improved accuracy in risk prediction for brain cancer, resulting in potential changes in patient management and follow-up protocols.
With the implementation of temporal learning models, researchers have noted a substantial improvement in prediction accuracy, marking a significant milestone in the fight against pediatric brain tumors. By leveraging large datasets of MRI scans taken over months, AI can recognize patterns that would otherwise go undetected in single-scan analyses. This innovation not only minimizes the anxiety associated with frequent imaging but also enhances the chances of catching a relapse early, thereby increasing the effectiveness of subsequent treatments. The implications of this technology extend beyond gliomas, presenting a paradigm shift applicable to various medical imaging scenarios.
Future Directions in Pediatric Cancer Management
As we look to the future of pediatric cancer management, the integration of advanced AI tools into routine clinical practice is poised to revolutionize care. The ongoing research at institutions like Mass General Brigham highlights the potential for AI to transform how clinicians assess relapse risks for pediatric gliomas. By moving beyond traditional, single-image methodologies, healthcare providers can harness the power of comprehensive predictive analytics to tailor treatment approaches to individual patient profiles, enhancing overall care.
Moreover, the prospect of clinical trials investigating AI-informed risk predictions offers exciting avenues to refine therapeutic strategies. By identifying at-risk patients early, clinicians could either reduce unnecessary imaging for lower-risk cases or initiate timely and targeted therapies for those deemed high-risk. This proactive shift in treatment planning not only boosts the chances of successful outcomes but also promotes a more personalized approach to pediatric cancer care, ultimately benefiting children battling brain tumors and their families.
The Impact of Recurrence on Families
The recurrence of pediatric gliomas can profoundly impact not only the affected children but also their families. The uncertainty surrounding the potential for relapse introduces significant emotional and psychological challenges for parents and siblings. As children undergo treatment, families often experience a cycle of hope and fear, particularly when their child’s recovery is uncertain. Understanding the role of pediatric glioma recurrence in family dynamics is crucial in providing holistic care that supports both the patient and their loved ones.
AI tools that enhance the prediction of pediatric cancer recurrence bring a new level of reassurance to families facing these daunting challenges. By providing more accurate assessments of relapse risks, families can engage with healthcare providers on informed levels about treatment options and management strategies. This partnership fosters a sense of empowerment and control, helping families cope with the uncertainties that accompany a childhood cancer diagnosis. Ultimately, advancements in technology not only aid in medical treatment but also play a vital role in addressing the psychosocial needs of patients and their families.
Advancements in Pediatric Cancer Treatment Protocols
Recent advancements in pediatric cancer treatments are heavily influenced by innovative technologies and research in AI and imaging techniques. The study leveraging temporal learning at Mass General Brigham exemplifies how the integration of advanced analytics leads to more effective treatment protocols. As we understand the correlation between imaging data and glioma relapse, treatment strategies can be optimized, potentially moving toward personalized care plans that cater to individual patient risks and histories.
This shift towards precision medicine in pediatric oncology is not just a response to the limitations of traditional treatments but is also a proactive approach to combating childhood brain cancer. As AI prediction tools become more commonplace, healthcare teams can develop tailored therapies that are not only more effective but also less invasive, minimizing the long-term repercussions of treatment on young patients. This evolution in pediatric cancer treatment strategies exemplifies a promising future where technology and compassionate care go hand in hand.
Enhancing Monitoring Practices in Pediatric Oncology
Effective monitoring of pediatric glioma patients is paramount in improving outcomes and ensuring timely interventions. Traditional follow-up practices often place a heavy emotional and physical burden on families, requiring frequent MRI scans and hospital visits. However, with the advent of AI and advanced imaging techniques, there is an opportunity to streamline these processes considerably. By utilizing predictive analytics, healthcare providers can create a more tailored monitoring approach that minimizes disruption while maximizing detection for potential recurrences.
The combination of AI tools and temporal learning methodologies provides a robust framework for enhancing monitoring practices. This evolution allows for a shift from reactive to proactive monitoring, where adjustments in imaging frequency can be based on a patient’s specific risk assessment. Children classified as low-risk may experience fewer MRI sessions, alleviating stress and providing families with a more manageable approach to care. Conversely, those categorized as high-risk can receive more frequent evaluations, ensuring they benefit from timely interventions. This balance represents a significant advancement in how pediatric cancer care is delivered.
AI and the Future of Pediatric Brain Cancer Research
The role of AI in pediatric brain cancer research is unlocking new possibilities for understanding tumor behaviors and responses to treatment. Ongoing studies reveal that using AI tools not only improves prediction accuracy for glioma recurrences but also contributes to a broader understanding of brain cancer dynamics in children. By analyzing large datasets and identifying patterns, researchers can develop insights that could potentially reshape existing treatment guidelines.
As the landscape of pediatric oncology becomes increasingly data-driven, collaborating across institutions can amplify the impact of AI research. Initiatives that gather extensive imaging data can fuel the development of sophisticated predictive models, ultimately leading to groundbreaking approaches in therapy and monitoring. By embracing AI as a pivotal component of pediatric cancer research, the medical community positions itself to revolutionize treatment and improve the prognoses for future generations of children diagnosed with brain tumors.
Frequently Asked Questions
What is pediatric glioma recurrence and how can it be detected early?
Pediatric glioma recurrence refers to the return of brain tumors in children, typically after initial treatment such as surgery. Early detection is crucial and can be enhanced by advanced methods like AI tools. Recent studies indicate that AI tools can analyze multiple brain scans over time, significantly improving the accuracy of predicting relapse risk compared to traditional imaging methods.
How does AI prediction improve the monitoring of brain cancer in children, particularly for glioma recurrence?
AI prediction tools enhance the monitoring of brain cancer in children by utilizing temporal learning methods to analyze a series of brain scans over time. This approach allows for the identification of subtle changes that may indicate the risk of glioma recurrence, ultimately leading to better long-term care and tailored treatment strategies.
What role does glioma risk assessment play in managing pediatric brain cancer?
Glioma risk assessment is vital in managing pediatric brain cancer as it helps identify patients at a higher risk of recurrence. The integration of AI-based models for risk assessment improves the precision of predictions, guiding clinicians in tailoring follow-up care and treatment interventions based on individual patient risk profiles.
What advancements have been made in pediatric cancer AI tools for predicting glioma relapse?
Recent advancements in pediatric cancer AI tools involve the application of temporal learning techniques that analyze multiple MRI scans over time. This approach significantly enhances the predictive accuracy for glioma relapse, achieving rates between 75-89%, as opposed to traditional methods based on single images, which offer much lower accuracy.
Why is temporal learning important in predicting pediatric glioma recurrence?
Temporal learning is important as it allows AI models to understand changes in brain scans sequentially over time, rather than in isolation. This method improves predictions of pediatric glioma recurrence by correlating observed changes in imaging with the likelihood of relapse, which could ultimately inform clinical decisions and patient care.
| Key Point | Description |
|---|---|
| AI Tool Development | Researchers developed an AI tool that predicts the risk of relapse in pediatric glioma patients by analyzing multiple brain scans over time. |
| Temporal Learning Method | The AI uses a technique called temporal learning, which synthesizes information from several scans taken over time rather than relying on single images. |
| Study Findings | The AI model achieved a prediction accuracy of 75-89% for glioma recurrence, significantly better than the 50% accuracy of single-image predictions. |
| Potential Benefits | This method can reduce the frequency of follow-up imaging for low-risk patients and offer targeted therapies for high-risk patients. |
| Next Steps | Further validation and clinical trials are needed to assess the real-world application of these AI-informed predictions. |
Summary
Pediatric glioma recurrence presents significant challenges for treatment, often leading to devastating outcomes after initial success. Recent advancements in AI technology now provide a promising tool to better predict recurrence risk, surpassing traditional methods. By analyzing multiple brain scans over time, researchers are enhancing predictive accuracy, ultimately aiming to improve care and reduce unnecessary stress on children and families. As the AI model undergoes further validation, it holds the potential to revolutionize follow-up care for pediatric glioma patients.