TIM-3 for Alzheimer’s treatment represents a groundbreaking approach that leverages the immune system’s capabilities to battle this debilitating disease. Recent studies have identified the TIM-3 molecule as a significant player in regulating the immune response in Alzheimer’s patients, particularly in relation to the activity of microglia, the brain’s primary immune cells. By inhibiting TIM-3, researchers have found that these microglial cells can be freed from their traditional roles, allowing them to effectively clear amyloid plaques that contribute to cognitive decline. This innovative strategy not only highlights the potential for immune system Alzheimer’s therapies but also opens new avenues for Alzheimer’s disease therapy that could enhance memory restoration. With the successful application of TIM-3 research, the prospects for treating Alzheimer’s—often linked with aging populations—could finally see more promising advancements.
The use of TIM-3 in treating Alzheimer’s disease offers a fascinating intersection between immunology and neurobiology. This checkpoint molecule, previously known for its implications in cancer treatment, has now been recognized for its role in Alzheimer’s pathology. Researchers are exploring how targeting TIM-3 can manipulate the immune response to enhance the brain’s ability to manage amyloid plaques and restore cognitive function. With promising results from animal studies, the emergence of TIM-3 as a focus in Alzheimer’s research could signify a new chapter in neural health strategies, ultimately aiming to reconfigure the immune system for better management of neurodegenerative conditions.
Exploring TIM-3’s Role in Alzheimer’s Treatment
Recent studies have illuminated the critical role that TIM-3 plays in the immune system’s response to Alzheimer’s disease. TIM-3, a checkpoint molecule, functions as an inhibitor that prevents microglia, the brain’s immune cells, from attacking harmful plaques comprised of amyloid beta. This interaction is particularly prevalent in patients with late-onset Alzheimer’s, where genetic variations linked to the TIM-3 gene, HAVCR2, have been identified as significant risk factors. By further understanding the mechanisms of TIM-3, researchers are hopeful that they can develop therapies that modulate its activity to enhance plaque clearance and improve cognitive function in those suffering from the disease.
The potential for TIM-3 to be repurposed from cancer therapies to Alzheimer’s treatments is an exciting frontier in clinical research. This strategy is particularly appealing given the limitations of current Alzheimer’s therapies, which have shown only minimal efficacy after numerous trials. By targeting TIM-3, scientists aim to unleash the innate capabilities of microglia to clear plaques from the brain, thereby not only improving cognitive function but also addressing the underlying neurodegenerative processes associated with the disease.
The Impact of Checkpoint Molecules on Alzheimer’s Disease Therapy
Checkpoint molecules such as TIM-3 are pivotal in regulating the immune response, ensuring that the body does not attack its own tissues. In the context of Alzheimer’s disease, this balance becomes skewed, as elevated TIM-3 levels inhibit microglia from performing their essential function of clearing amyloid plaques. This failure leads to a buildup of toxic substances in the brain, contributing to cognitive decline and memory loss associated with Alzheimer’s. As scientists explore the intricate relationship between immune regulation and Alzheimer’s, the manipulation of TIM-3 offers a promising therapeutic avenue to restore immune functionality.
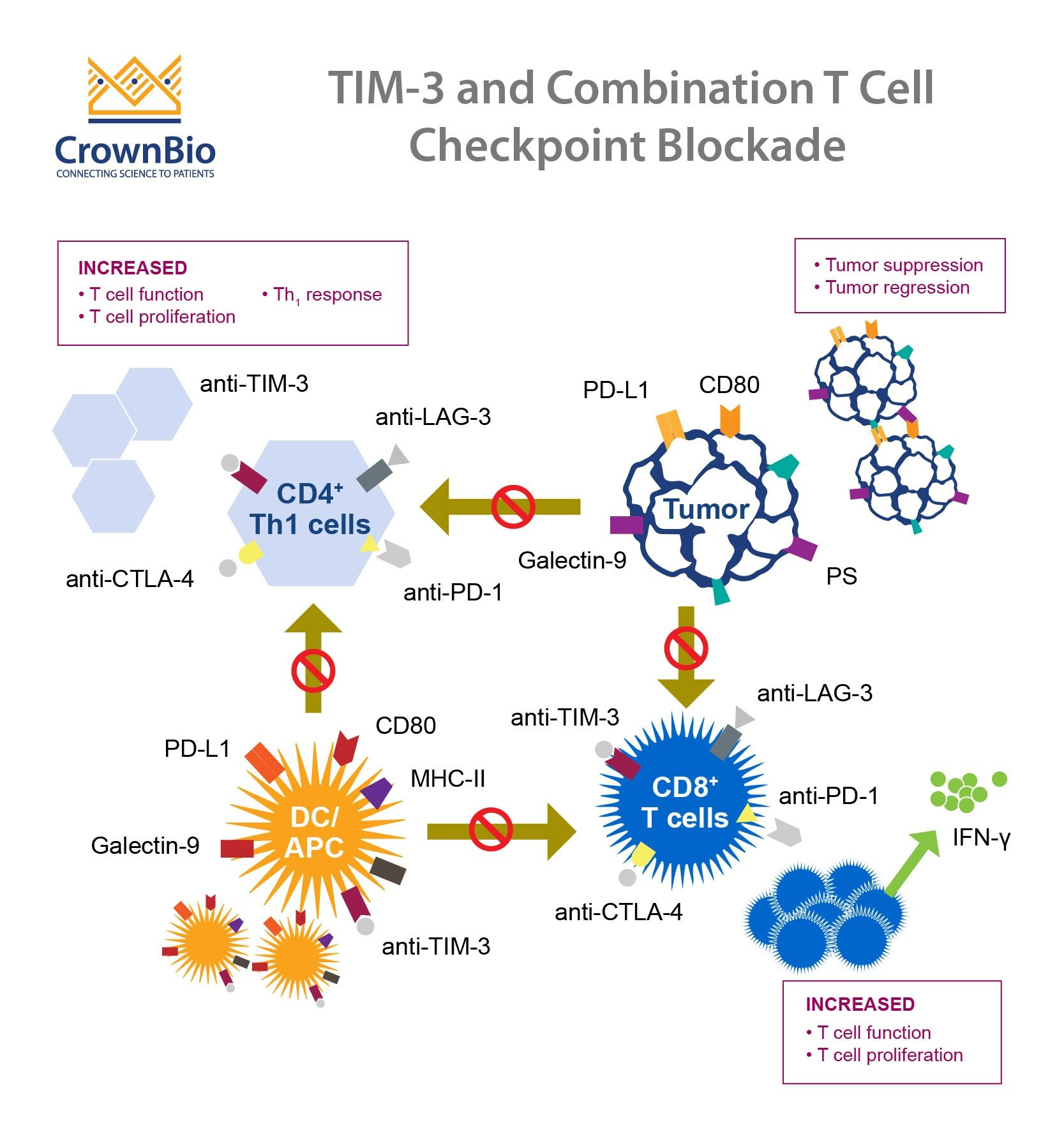
Innovative therapeutic approaches that leverage checkpoint molecules are on the horizon. Targeting TIM-3 through specific inhibitors such as anti-TIM-3 antibodies could create a breakthrough in Alzheimer’s treatment. These therapies would potentially revive the microglial function necessary for plaque clearance and offer a dual benefit by minimizing the neuroinflammation that exacerbates Alzheimer’s pathology. By honing in on the immune system and its checkpoints, researchers strive to develop effective treatments that can provide significant cognitive improvements for those battling Alzheimer’s.
Microglia and Their Functions in Alzheimer’s Disease
Microglia are the brain’s resident immune cells and play an essential role in maintaining neurological health. They are responsible for pruning synapses during brain development, which is crucial for optimal memory function. However, in older adults and those with Alzheimer’s disease, microglia become dysregulated and exhibit increased expression of TIM-3, turning them from active plaque-clearers into cells that merely maintain homeostasis. This change hampers their ability to effectively remove amyloid beta plaques, leading to further cognitive impairment and memory issues.
The dual role of microglia and their interaction with the TIM-3 checkpoint molecule presents a complex challenge in Alzheimer’s research. While microglia are designed to protect and prune unnecessary neural connections, their failure to clear amyloid plaques signifies a dysfunction that could be the key to unlocking new treatments. By understanding how TIM-3 modulates their activity, researchers can devise strategies to shift microglia back to their protective roles, which could ultimately lead to groundbreaking approaches in the therapeutic management of Alzheimer’s disease.
Understanding Amyloid Plaques and Their Impact on Memory
Amyloid plaques, characteristic of Alzheimer’s disease, are detrimental aggregates that form in the brains of affected individuals. These plaques are formed when amyloid beta peptides accumulate, leading to neurotoxicity and a decline in cognitive function. In healthy brains, microglia are equipped to clean up these plaques, but the inhibitory effect of molecules like TIM-3 stymies this process. As a result, the presence of amyloid plaques enhances neuroinflammation and accelerates the progression of Alzheimer’s, creating a vicious cycle that greatly affects memory and learning.
The accumulation of amyloid plaques and the subsequent failure of microglial clearance are central to the pathological progression of Alzheimer’s. Increasing evidence suggests that therapies targeting TIM-3 may restore the microglia’s ability to recognize and engulf these toxic aggregates, thereby mitigating memory loss and cognitive decline. By unraveling the mechanisms governing amyloid plaque formation and clearance, scientists are optimistic that interventions can be crafted to break this cycle and restore cognitive function in Alzheimer’s patients.
The Relationship Between TIM-3 and Cognitive Function
Recent findings from research involving TIM-3 demonstrate a direct correlation between the activity of this checkpoint molecule and cognitive function in Alzheimer’s disease. In laboratory models, the deletion of the TIM-3 gene in mice led to enhanced clearance of amyloid plaques, correlating with improvements in memory and cognitive behavior. These behavioral assessments showcase the critical link between immune modulation and cognitive health, suggesting that therapies aimed at reducing TIM-3 expression could yield substantial benefits in the management of Alzheimer’s.
Moreover, the understanding that TIM-3 can both inhibit and enhance microglial activity presents a nuanced approach to Alzheimer’s therapy. Balancing TIM-3 levels could be crucial in restoring not only the microglial function but also improving overall cognitive functions. Continued research efforts into TIM-3’s roles promise to pave the way for innovative treatments that can target the immune dysfunction seen in Alzheimer’s, ultimately benefiting those with cognitive impairments.
Innovations in Alzheimer’s Disease Research and Treatment
The field of Alzheimer’s research is at a pivotal moment, especially with the introduction of new therapeutic approaches focused on immune modulation. One promising avenue is the use of TIM-3 inhibitors to rejuvenate microglial activity against amyloid beta plaques. As traditional treatments have yielded incremental results, exploring immune system interactions can offer fresh hope for patients. This innovative perspective could catalyze a new era in Alzheimer’s disease therapies, enhancing clearance of neuropathological constructs that severely impair memory.
Innovations inspired by cancer therapies are encouraging as they reveal new therapeutic strategies for Alzheimer’s disease. Researchers are now investigating existing anti-TIM-3 antibodies, previously developed for cancer treatment, for their potential adaptation in targeting Alzheimer’s pathology. By applying strategies that have been successful in oncological contexts, scientists aim to unlock new avenues for effectively addressing the complexities inherent in Alzheimer’s disease, ultimately aiming for substantial neuroprotection and improved quality of life for patients.
The Challenges of Targeting Plaque Formation in the Brain
Despite the promising avenue of targeting TIM-3 to enhance microglial activity, challenges remain in effectively clearing amyloid plaques from the brain. The relationship between TIM-3 expression and plaque accumulation underscores a complex dynamic that requires careful navigation in therapy development. Ethically, researchers must consider the delicate balance of enhancing immune function without overstimulating the immune response, which can lead to unwanted neuroinflammation and further cognitive decline.
Additionally, while targeting TIM-3 and its mechanisms holds promise, the multifactorial nature of Alzheimer’s disease means that a one-size-fits-all approach may not suffice. Future therapeutic strategies may need to integrate TIM-3 modulation with other methods aimed at addressing comprehensive aspects of Alzheimer’s, from neuroinflammation to other non-amyloid-related factors. This holistic approach could ultimately yield more successful outcomes in future clinical interventions.
Future Directions in TIM-3 Research for Alzheimer’s
Looking ahead, the future of TIM-3 research in Alzheimer’s therapy appears promising but requires further exploration. Studies that translate findings from mouse models to human applications will be critical to understand the therapeutic potential truly. As researchers assess the effectiveness of anti-TIM-3 therapies in halting plaque development, the overarching goal is to catalyze significant cognitive improvements in patients diagnosed with Alzheimer’s disease.
Moreover, understanding the complete role of TIM-3 in the brain’s immune response will be essential not only for developing targeted treatments but also for anticipating possible side effects. Ongoing research must continue to refine and adjust the therapeutic frameworks within which TIM-3 inhibitors are utilized, ensuring that they provide maximum benefit while minimizing any adverse effects. The intricacies of TIM-3’s role in immunology and Alzheimer’s pathology beckon a rigorous investigative journey that could redefine therapeutic landscapes.
Collaboration and Funding in Alzheimer’s Research
Successful research endeavors often rely on collaborative efforts, and this holds particularly true in the context of Alzheimer’s disease studies. The collaboration between different institutes, as seen in the research spearheaded by Vijay Kuchroo and his colleagues, serves as a model for how multidisciplinary approaches can enhance understanding and effectiveness in therapeutic development. Such partnerships bring together diverse expertise needed to tackle the complexities of Alzheimer’s and facilitate the translation of novel concepts such as TIM-3 target therapies into tangible treatments.
Funding also plays a crucial role in propelling Alzheimer’s research forward. Institutions like the National Institutes of Health (NIH) provide necessary resources that enable researchers to conduct in-depth studies while fostering innovation in therapeutic approaches. As interest in Alzheimer’s disease continues to rise, along with the understanding of its immunological aspects, the allocation of increased research funding will be vital for advancing promising strategies like TIM-3 modulation and ensuring their progression from laboratory settings to clinical applications.
Frequently Asked Questions
What is TIM-3 and how does it relate to Alzheimer’s treatment?
TIM-3 is an immune checkpoint molecule that plays a critical role in the immune response by inhibiting the activity of immune cells, particularly microglia in the brain. Recent research indicates that TIM-3 contributes to the accumulation of amyloid plaques in Alzheimer’s disease by preventing microglia from clearing these damaging proteins. Targeting TIM-3 may enhance the immune response against plaques and represent a promising strategy for effective Alzheimer’s disease therapy.
How does TIM-3 affect microglia and their function in Alzheimer’s disease?
In Alzheimer’s disease, TIM-3 is overexpressed on microglia, the brain’s immune cells, which inhibits their ability to engulf and clear amyloid-beta plaques. This lack of clearance contributes to plaque accumulation and cognitive decline. By blocking TIM-3, researchers have shown that microglia can regain their ability to eliminate plaques, thus potentially restoring cognitive function in Alzheimer’s models.
What are the potential treatment options involving TIM-3 for Alzheimer’s patients?
Potential treatment options may include the use of anti-TIM-3 antibodies or small molecules designed to inhibit TIM-3’s effects on microglia. These therapies aim to restore microglial function, allowing them to effectively attack and clear amyloid plaques from the brain, thereby providing a novel approach to Alzheimer’s disease therapy.
Why is TIM-3 considered a breakthrough in Alzheimer’s disease research?
TIM-3 is a breakthrough in Alzheimer’s research because it links the immune system to the disease’s pathology. By targeting this specific checkpoint molecule, researchers could potentially modify the course of Alzheimer’s by enhancing the brain’s immune response, leading to improved plaque clearance and better cognitive outcomes.
Can TIM-3 therapies be used for other conditions beyond Alzheimer’s treatment?
Yes, while TIM-3 therapies are primarily focused on Alzheimer’s disease, they could also have implications for other conditions where microglial dysfunction plays a role, such as multiple sclerosis or traumatic brain injury. Additionally, since TIM-3 is also targeted in cancer therapies, there may be opportunities to explore its applications in enhancing immune responses across various diseases.
What evidence supports the role of TIM-3 in Alzheimer’s disease?
Research has shown that TIM-3 genetic polymorphisms are linked to increased risk for late-onset Alzheimer’s disease. Experimental studies using genetically modified mice demonstrated that deleting the TIM-3 gene leads to reduced amyloid plaque accumulation and improved cognitive function, reinforcing the molecule’s critical role in Alzheimer’s pathology.
How long has the research on TIM-3 for Alzheimer’s been conducted?
The research on TIM-3 as a potential therapeutic target for Alzheimer’s disease has been ongoing for approximately five years. This extensive research includes various experimental studies to elucidate the mechanisms by which TIM-3 affects microglial function and plaque clearance in the brain.
What are microglia and why are they important in Alzheimer’s disease?
Microglia are the primary immune cells of the brain, responsible for maintaining homeostasis and clearing cellular debris, including amyloid plaques associated with Alzheimer’s disease. Their ability to efficiently phagocytose harmful substances is essential for brain health. In Alzheimer’s, their dysfunction, exacerbated by factors like TIM-3, contributes to the progression of the disease.
How does TIM-3 therapy differ from current Alzheimer’s treatments?
Unlike current therapies, which often focus on amyloid-beta alone, TIM-3 therapy aims to restore immune function directly, allowing microglia to effectively clear plaques and potentially improve cognitive symptoms. This approach represents a shift towards enhancing the brain’s own defenses rather than solely targeting plaque accumulation.
| Key Point | Details |
|---|---|
| Introduction of TIM-3 in AD | Research shows TIM-3, a checkpoint molecule, may help treat Alzheimer’s by enabling microglia to clear amyloid plaques. |
| Role of Microglia | Microglia are brain immune cells that prune synapses during development but fail to clear plaques in Alzheimer’s due to TIM-3. |
| Genetic Link | TIM-3 is linked to late-onset Alzheimer’s, with genetic polymorphism increasing its expression on microglia in patients. |
| Impact of TIM-3 Deletion | Deleting TIM-3 in mice enhances plaque clearance and improves cognitive function, indicating potential for therapy. |
| Therapeutic Applications | Theoretical therapy would work using an anti-TIM-3 antibody to inhibit the function of TIM-3 and boost microglial activity. |
| Future Prospects | Research is ongoing to test human anti-TIM-3 antibodies for their efficacy in combating amyloid plaque development in AD. |
Summary
TIM-3 for Alzheimer’s treatment represents a promising new direction in combating this debilitating disease. By targeting the TIM-3 checkpoint molecule, researchers have uncovered a method to enhance the brain’s immune response, enabling microglial cells to effectively clear harmful amyloid plaques. This breakthrough opens new avenues for therapeutic interventions, leveraging a strategy historically successful in cancer treatment to potentially restore cognitive function in Alzheimer’s patients.