Maternal mortality in the U.S. is a troubling issue that continues to rise, placing the nation at the top of the list among high-income countries for pregnancy-related deaths. A study reveals that more than 80% of these fatalities are preventable, yet systemic flaws in the healthcare system contribute to persistent maternal health issues. Disparities based on race, ethnicity, and geography further complicate the landscape, with American Indian and Alaska Native women experiencing nearly four times the mortality rate of their white counterparts. Chronic health conditions, such as hypertension, are increasingly impacting younger individuals, raising alarms among healthcare professionals. To combat these startling statistics, there is a pressing need for better prenatal and postpartum care, as well as targeted policies that address healthcare disparities within maternal health.
The alarming trend of increased maternal death rates in the U.S. speaks to a broader crisis in reproductive health and care. With a significant number of pregnancy-related fatalities classified as preventable, it is crucial to address the underlying healthcare disparities that disproportionately affect women of color and those from rural communities. Chronic illnesses, including cardiovascular issues, have emerged as leading contributors to this public health dilemma, particularly among younger mothers. Advancements in postpartum care and a more inclusive approach to maternal well-being are urgently needed to improve outcomes for mothers across all demographics. As the maternal health landscape evolves, recognizing the continuum of care needed extends beyond pregnancy and into the critical months following childbirth.
Understanding Maternal Mortality in the U.S.
Maternal mortality remains a significant public health concern in the United States, with the nation leading all high-income countries in this alarming statistic. The prevalence of pregnancy-related deaths underscores the urgent need for comprehensive prenatal and postpartum care. Studies show that over 80% of these deaths are preventable yet continue to rise due to a myriad of factors, including chronic health conditions and systemic healthcare disparities. It is imperative to analyze the underlying causes of these maternal health issues, from inequitable access to quality healthcare to the prevalence of chronic illnesses such as hypertension and cardiovascular disease that disproportionately affect expectant mothers.
Inequities in maternal health outcomes have been highlighted by new research revealing significant disparities across racial and ethnic groups. American Indian and Alaska Native women face nearly four times the mortality rate of their white counterparts. These disparities indicate a broader systemic issue within the healthcare system, characterized by biases and a lack of targeted resources for marginalized communities. Addressing these disparities requires a multi-faceted approach that includes policy reform, enhanced training for healthcare providers, and improved access to comprehensive maternal care services.
The Role of Chronic Health Conditions in Maternal Health
Chronic health conditions play a critical role in maternal health outcomes, impacting both pregnancy and postpartum recovery. Conditions such as hypertension and diabetes are increasingly prevalent among women of reproductive age, highlighting a concerning trend that necessitates urgent attention. The transition from hemorrhage to cardiovascular disease as the leading cause of pregnancy-related deaths reflects the growing incidence of these chronic issues within the population. This rise is associated with younger age groups experiencing serious health conditions, traditionally seen in older populations, pointing to a need for better monitoring and management of women’s health prior to and during pregnancy.
To mitigate the risks associated with chronic health conditions, it is crucial to implement robust screening and management programs within healthcare systems. Early identification of at-risk women through improved access to prenatal care can help manage chronic conditions before they escalate during pregnancy. Moreover, integrating maternal health education into primary care practices can empower women with knowledge about their health and the risks associated with certain conditions. Ultimately, by addressing these chronic health issues, we can significantly reduce the rates of maternal mortality and enhance overall maternal health outcomes.
The Importance of Enhanced Postpartum Care
Frequently Asked Questions
What factors contribute to the high maternal mortality rate in the U.S. compared to other high-income countries?
The U.S. has the highest maternal mortality rate among high-income nations due to various factors, including a fragmented healthcare system, inequitable policies, maternity care deserts, and persistent bias in healthcare. Additionally, increasing rates of chronic health conditions, such as cardiovascular diseases among the reproductive age population, contribute significantly to pregnancy-related deaths.
How does race and ethnicity affect maternal mortality in the U.S.?
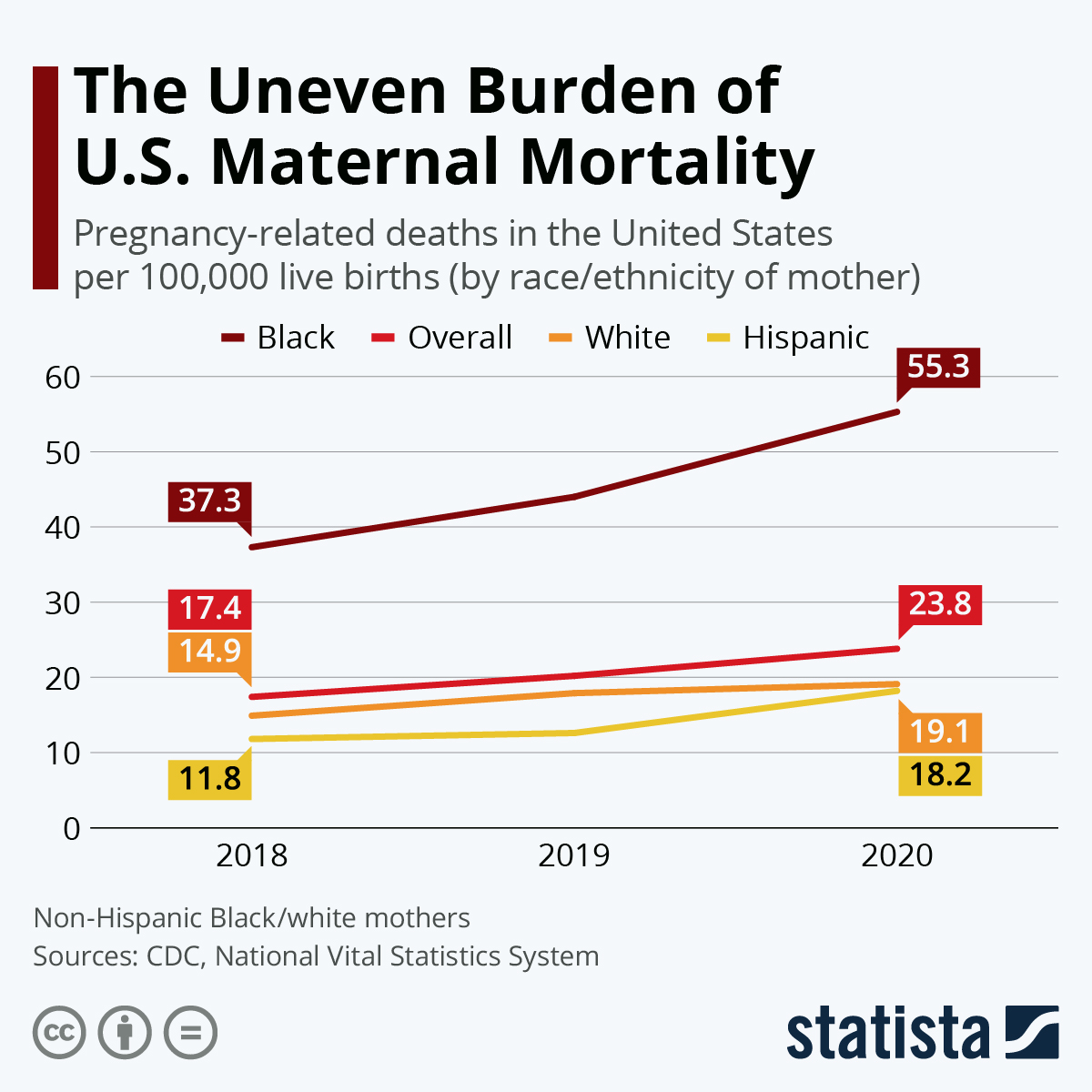
Maternal mortality rates in the U.S. show significant disparities across racial and ethnic groups. For instance, American Indian and Alaska Native women face the highest mortality rate, nearly four times that of white women. Non-Hispanic Black women also have a disproportionately high risk. These disparities highlight systemic issues in maternal health and the importance of addressing healthcare inequalities.
What role does postpartum care play in reducing maternal mortality rates?
Postpartum care is crucial in reducing maternal mortality because a significant number of pregnancy-related deaths occur after the delivery, often in the postpartum period. Improving healthcare systems to provide extended support and resources in the months following childbirth is essential to prevent late maternal deaths and ensure comprehensive care during this critical time.
How has the COVID-19 pandemic affected maternal mortality rates in the U.S.?
The COVID-19 pandemic has exacerbated existing maternal health issues, contributing to a rise in pregnancy-related deaths. The sharp increase in mortality rates observed in 2021 corresponds to the pandemic’s impact, as healthcare disruptions and increased stressors on the healthcare system likely affected maternal care and outcomes.
Why is the definition of maternal mortality important in discussing U.S. health issues?
Defining maternal mortality is crucial because it frames the healthcare response and public health strategies. While the World Health Organization defines maternal mortality as deaths occurring during pregnancy and up to 42 days postpartum, a growing recognition of late maternal deaths (up to one year after childbirth) emphasizes the need for continuous postpartum care and monitoring.
What interventions are necessary to reduce preventable pregnancy-related deaths in the U.S.?
To reduce preventable pregnancy-related deaths, the U.S. must invest in enhancing healthcare infrastructure, particularly improving access to quality prenatal and postpartum care. Addressing chronic health conditions, eliminating healthcare disparities, and implementing evidence-based policy changes can also lead to significant improvements in maternal health outcomes.
| Key Point | Details |
|---|---|
| Preventable Deaths | More than 80% of pregnancy-related deaths in the U.S. are preventable. |
| Maternal Mortality Rate | The U.S. leads high-income countries in maternal mortality with rising rates between 2018 and 2022. |
| Racial Disparities | American Indian and Alaska Native women face the highest mortality rates, significantly more than white women. |
| Leading Cause of Death | Cardiovascular diseases have become the leading cause of pregnancy-related deaths, surpassing hemorrhages. |
| Late Maternal Deaths | Late maternal deaths account for nearly a third of total pregnancy-related deaths, deserving more focus and improved care. |
| Public Health Infrastructure | Investment in public health resources and maternal care is crucial to reversing the trend of rising maternal mortality. |
Summary
Maternal mortality in the U.S. has reached alarming rates, continuing to rise among high-income countries. Despite the fact that over 80% of these deaths are preventable, systemic issues within the healthcare infrastructure, significant racial disparities, and rising chronic health conditions contribute to this ongoing crisis. Addressing these issues requires a multifaceted approach, including improving access to quality prenatal and postpartum care, especially for high-risk populations. Effective strategies and investments in maternal health infrastructure are imperative to reversing the current trajectory and improving outcomes for mothers across the nation.