Alzheimer’s disease research is at the forefront of tackling one of the most pressing neurodegenerative diseases affecting millions worldwide. Pioneering scientists like Beth Stevens are uncovering critical roles played by microglial cells, which function as the brain’s immune system, combating neurodegeneration while also clearing damaged cells. These revelations shed light on the delicate balance of synaptic pruning, revealing how dysfunctional processes can lead to Alzheimer’s and other related disorders. The implications of this research are vast, potentially leading to groundbreaking Alzheimer’s treatments and early detection biomarkers that could transform patient care. With nearly 7 million Americans already facing this challenge, Stevens and her team’s work could help shape a brighter future for those living with Alzheimer’s.
Exploring advancements in Alzheimer’s disease exploration highlights exciting developments in understanding this dementia and its impact on brain health. Research led by innovative scholars, such as Beth Stevens, focuses on brain immune mechanisms, particularly the activity of microglial cells, offering new insights into their role in neuroinflammation. As scientists delve deeper into the dynamics of how these cells respond to neurodegenerative conditions, they pave the way for potential therapies that could mitigate symptoms or even halt progression. This line of inquiry bridges fundamental science and potential clinical applications, presenting opportunities for earlier diagnoses and more effective interventions for Alzheimer’s and related cognitive decline. In a world where the aging population is rapidly increasing, such research is not only timely but critical for improving outcomes in brain health.
Revolutionizing Alzheimer’s Disease Research
Alzheimer’s disease research has seen a monumental shift as scientists like Beth Stevens challenge long-standing beliefs about the brain’s immune system, specifically focusing on microglial cells. These cells, which are essential for maintaining brain health by clearing away debris and modulating synaptic connections, are now being recognized for their potential link to Alzheimer’s and other neurodegenerative diseases. Stevens’ work at the Stevens Lab has opened new avenues in understanding how improper functions of these cells can exacerbate disease progression, paving the way for innovative treatment options.
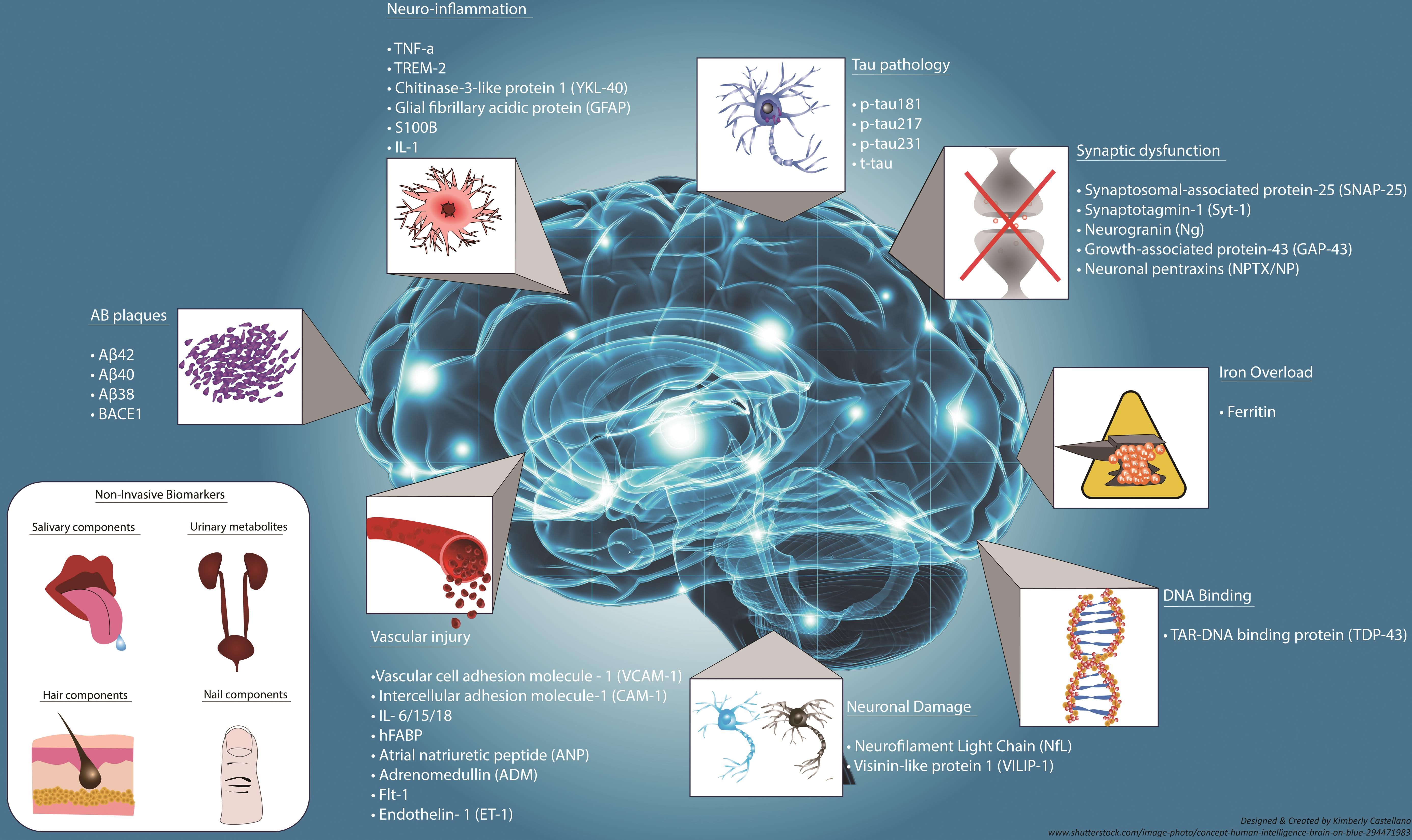
The significance of Stevens’ research lies not only in unraveling the complexities of microglial functionality but also in enhancing early detection methodologies for Alzheimer’s. By identifying biomarkers associated with abnormal microglial activity, researchers can potentially diagnose the disease much earlier in its course, enabling timely intervention. This proactive approach can significantly enhance the quality of life for the millions affected by Alzheimer’s, and Stevens’ findings emphasize the critical need for a multidisciplinary effort in Alzheimer’s treatment advancements.
Understanding Microglial Cells: The Brain’s Immune Guardians
Microglial cells play a pivotal role as the brain’s primary immune defenders, constantly surveilling the neural environment for signs of distress. Instead of being mere support cells, they actively participate in synaptic pruning, a process vital for normal brain function and development. However, Stevens’ research has illuminated a darker aspect of this pruning process; when microglia become dysregulated, they can contribute to neurodegenerative diseases like Alzheimer’s, thereby highlighting their dual role in promoting health and causing disease.
The complexities surrounding microglial function have significant implications for therapeutic strategies aimed at combating Alzheimer’s disease. Understanding how these immune cells interact with neurons and contribute to synaptic degeneration not only sheds light on the pathophysiology of neurodegenerative diseases but also opens up potential targets for drug development. With Stevens leading the charge, the research emphasizes the need for continued investigation into brain immunity and its relationship with diseases such as Alzheimer’s.
Beth Stevens: Driving Force in Neuroscience Innovation
Beth Stevens has established herself as a transformative figure in the realm of neuroscience, particularly through her innovative work with microglial cells. Her journey reflects a commitment to scientific inquiry fueled by curiosity and driven by a desire to uncover the underlying mechanisms of metabolic disorders and brain diseases. Stevens emphasizes the importance of fundamental science, asserting that her research is built on the foundational knowledge gained over years of inquiry, primarily supported by federal health investments.
Recognized for her contributions with accolades such as the MacArthur ‘genius grant,’ Stevens embodies the spirit of scientific exploration that seeks to translate basic research into applicable solutions for devastating illnesses like Alzheimer’s. Her belief that insights gained in model organisms can lead to paradigmatic shifts in understanding human diseases positions her work at the forefront of modern neuroscience, inspiring future generations of scientists to explore the complexities of the brain’s immune system.
The Role of Research Funding in Neurodegenerative Disease Studies
The pursuit of breakthroughs in Alzheimer’s disease research often hinges on robust funding sources, particularly from government institutions like the National Institutes of Health (NIH). Beth Stevens attributes the progress in her lab largely to the foundational support received from federal grants, which enables researchers to delve into complex scientific questions that may not immediately translate into clinical applications. This funding underscores the significance of curiosity-driven science in making strides against neurodegenerative diseases.
As the number of people living with Alzheimer’s grows, projected to double by 2050, the need for sustained investment in research becomes increasingly apparent. The financial backing not only propels innovative studies into microglial behavior and their implications for neurodegenerative diseases but also provides researchers with the resources to develop novel therapeutic strategies. Ensuring that research receives adequate funding is crucial for moving beyond basic inquiry into tangible improvements in Alzheimer’s treatment.
Innovations in Alzheimer’s Biomarkers through Microglial Research
Recent advances in Alzheimer’s research have increasingly focused on developing reliable biomarkers that can facilitate early diagnosis and intervention. Beth Stevens’ groundbreaking studies on microglial cells offer promise in identifying such biomarkers, as these immune cells exhibit distinct patterns of activity that change with the onset of neurodegenerative diseases. By examining the role of microglia in synaptic pruning, researchers aim to uncover specific indicators that signal the progression toward Alzheimer’s, thereby enabling preclinical interventions.
With the identification of new biomarkers derived from microglial activity, healthcare professionals can potentially monitor disease stages more effectively, tailoring treatments to individual patient needs. This shift toward precision medicine reflects the growing understanding of Alzheimer’s as a complex, multi-faceted disease, requiring comprehensive approaches that involve exploring the brain’s immune system. Stevens’ contributions to this field signify a crucial advancement toward reframing Alzheimer’s treatment protocols using early detection methods linked to microglial function.
Exploring Neurodegenerative Disease Mechanisms
The study of neurodegenerative diseases, particularly Alzheimer’s, requires a deep dive into the multifaceted mechanisms that underlie brain pathologies. Researchers like Beth Stevens are helping to unravel these mechanisms by examining the interactions between microglial cells and neurons, revealing how dysregulation of the immune response can lead to various cognitive impairments and degenerative conditions. Such insights are critical for creating comprehensive models that explain disease progression on both cellular and systemic levels.
Understanding the intricate dynamics of microglial involvement in synaptic integrity can offer valuable lessons for developing therapeutic strategies aimed at neurodegenerative diseases. Stevens’ research highlights the necessity for interdisciplinary collaboration to decode the complexities of Alzheimer’s pathology. This multi-layered exploration serves as a stepping stone toward innovative treatments that target the root causes of neurodegeneration, ultimately working toward a future where the burden of Alzheimer’s can be alleviated.
The Future of Alzheimer’s Treatment: A New Paradigm
As Alzheimer’s disease continues to impact millions, the future of treatment lies in innovative research like that of Beth Stevens, which focuses on the brain’s immune system and microglial cells. By shifting the paradigm from merely managing symptoms to understanding underlying mechanisms, researchers are identifying new targets for therapeutic intervention. This transformative approach represents a crucial turn in Alzheimer’s treatment strategies, offering hope for those affected by this challenging disease.
With the ongoing exploration of the link between microglial dysregulation and neurodegenerative disease, there is potential for creating more effective Alzheimer’s treatments that address the disease’s root causes. By encouraging the immune cells to function properly once more, scientists aim to restore balance within the brain, thereby preventing cognitive decline before it begins. Such advancements signify a promising shift in how we tackle Alzheimer’s, emphasizing the need for continuous research and innovation in the years to come.
Impact of Aging on Alzheimer’s Disease Progression
Aging is a significant factor in the progression of Alzheimer’s disease, influencing both disease onset and severity. As the population ages, the prevalence of neurodegenerative diseases is set to increase dramatically, with projections indicating that the number of cases will reach staggering figures by 2050. The work of researchers like Beth Stevens sheds light on how age-related changes in microglial function may contribute to the development and progression of Alzheimer’s disease, necessitating urgent attention to this growing public health crisis.
Understanding how aging affects microglial activity is crucial for devising effective interventions for older adults who are at risk of developing Alzheimer’s. Research indicates that age-related dysregulation of the brain’s immune response can lead to increased susceptibility to neurodegenerative processes. Targeting these age-related changes in microglial function may offer new avenues for preventing or slowing down the progression of Alzheimer’s in an aging population, making it imperative for continued investigations into the interaction between age, microglial cells, and Alzheimer’s pathology.
The Importance of Basic Science in Alzheimer’s Research
Basic science serves as the cornerstone for applied research, unlocking the fundamental principles that govern disease mechanisms. Beth Stevens emphasizes the importance of such exploratory work in her studies on microglial cells, which was foundational in establishing a clearer understanding of their role in neurodegenerative diseases like Alzheimer’s. Her journey illustrates the intricate relationship between curiosity-driven investigations and meaningful advancements in medical science, allowing researchers to uncover novel pathways for treatment and intervention.
Investing in basic science is critical for driving forward innovative solutions to combat Alzheimer’s disease. Understanding the cellular and molecular underpinnings of microglial dysfunction provides the basis for translating these findings into therapeutic strategies that can improve outcomes for those affected by Alzheimer’s. By continuing to support fundamental research, the scientific community can pave the way for breakthroughs that not only enhance our grasp of neurodegeneration but also lead to the development of effective treatments.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s disease research?
Microglial cells are crucial components of the brain’s immune system and play a significant role in Alzheimer’s disease research. They help to clear dead or damaged cells and prune synapses, but when their functioning is disrupted, it can lead to neurodegenerative diseases like Alzheimer’s. Recent research by Beth Stevens highlights how abnormal microglial pruning may contribute to the onset and progression of Alzheimer’s, and understanding this process opens avenues for new treatments.
How are neurodegenerative diseases linked to the findings of Beth Stevens in Alzheimer’s disease research?
Beth Stevens’ research on microglial cells has revealed significant connections between neurodegenerative diseases and immune system functions in the brain. Her findings indicate that improper synaptic pruning by microglia can lead to conditions such as Alzheimer’s and Huntington’s disease. This insight is pivotal in Alzheimer’s disease research as it points toward new strategies for treatment and intervention based on the underlying immune processes.
What innovations in Alzheimer’s treatment are emerging from microglial research?
Innovations in Alzheimer’s treatment are emerging from research on microglial cells, particularly from the Stevens Lab. By understanding how these cells contribute to disease processes, researchers are developing new therapeutic agents aimed at modulating microglial activity. This represents a shift towards targeting the brain’s immune response to improve Alzheimer’s treatment outcomes and potentially altering the disease’s progression.
How does the brain immune system impact Alzheimer’s disease research?
The brain immune system, primarily mediated by microglial cells, has a profound impact on Alzheimer’s disease research. Researchers like Beth Stevens are investigating how the immune response in the brain can both protect and damage neuronal health. Insights from this research are crucial for understanding the pathophysiology of Alzheimer’s and for creating biomarkers that can detect the disease earlier, improving prospects for treatment.
What future directions are anticipated in Alzheimer’s disease research based on current findings?
Future directions in Alzheimer’s disease research are likely to focus on the neuroimmune interactions mediated by microglial cells. Current findings suggest a need for further exploration of how these cells influence neurodegenerative processes and their potential as therapeutic targets. As new biomarkers are developed, researchers hope to improve early detection and develop more effective Alzheimer’s treatments tailored to individual immune responses.
| Key Points | Details |
|---|---|
| Research Focus | Beth Stevens researches microglial cells, which are crucial to the brain’s immune system. |
| Microglial Function | These cells patrol the brain, clearing damaged cells and pruning synapses. |
| Implications for Alzheimer’s | Research shows that abnormal microglial pruning may contribute to Alzheimer’s and other neurodegenerative diseases. |
| Funding and Support | Stevens emphasizes the importance of federal funding for advancements in her research. |
| Future of Research | The findings could lead to new medicines and earlier detection of Alzheimer’s. |
| Population Impact | With an aging population, Alzheimer’s cases are expected to double by 2050. |
Summary
Alzheimer’s disease research is at a pivotal point, with scientists like Beth Stevens paving the way for revolutionary discoveries in understanding the brain’s immune responses. By studying microglial cells, Stevens has uncovered how their normal functions can become detrimental in Alzheimer’s, opening new avenues for treatment and early diagnosis. As research continues to evolve, it is crucial for both public and private sectors to support innovative studies that could dramatically change the landscape of care and treatment for millions affected by Alzheimer’s.